How the Pandemic Is Making the Opioid Crisis Worse
- Get link
- X
- Other Apps
How the Pandemic Is Making the Opioid Crisis Worse
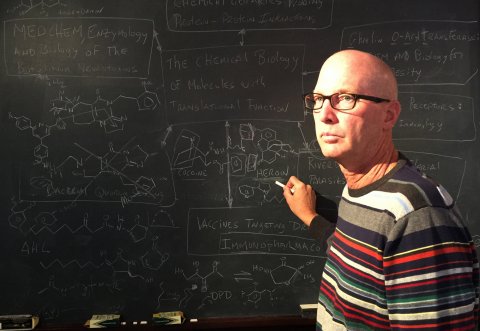
Kim Janda likes to say he has engineered immune cells in the lab capable of protecting the human body against virtually "everything that's walked or crawled"—including some of the most toxic known diseases, including anthrax, botulinum neurotoxin, and ricin. When someone close to Janda developed a drug addiction, it was only natural that the Scripps Research Institute scientist would try to help. Might it be possible, he wondered, to create a pill or a shot that could protect addicts from the consequences of their slips, by neutralizing the drug before it could get them high or cause an overdose? That way, it might be possible to keep addicts from relapsing, which sometimes proves fatal.
The need for such an intervention is more urgent than ever. Addiction has claimed 750,000 lives since 1999, according to the Centers for Disease Control. This year, COVID-19-related developments are adding to the downward spiral. Over the last three to four months overdose deaths have increased nationwide by close to 15 percent, says Shawn Ryan, Chair of Legislative Advocacy for the American Society of Addiction Medicine. Ryan is also president and chief medical officer of BrightView Health, a 20-site treatment network in Ohio and Kentucky, long considered ground zero for the nation's devastating opioid epidemic. So far this year, overdose deaths in the counties where his centers are located are up more than 25 percent, he says. The cause of this increase is no mystery. "If you write down a list of things that will make mental health and addiction worse in society or in a community," Ryan says, "COVID caused almost all of them—social isolation, economic instability, transportation disruption and challenges to getting support, anxiety related to social isolation—everything that would make our mental health and addiction crisis worse."
Janda had spent his career finding ways to harness the body's own immune system—and create things that mimicked it—to attack and neutralize the small molecules that cause disease. In the early 1990s, he set out to apply those same techniques to neutralize the effects of street drugs like heroin, cocaine and methamphetamine. "Addiction is a brain disease," he says. "The complexity of the brain chemistry involved is extremely difficult to target with a drug. But if you have a good enough antibody, it acts like a vacuum cleaner. It can suck the drug out of the brain."
In all this time, despite constant funding challenges—Janda reckons he's gotten a total of about $25 million in federal financing for his addiction vaccines, compared to billions for other vaccines, such as COVID-19—he and his ever-shifting research team have managed to create promising vaccines for some of the worst addiction scourges, including cocaine, amphetamine, heroin, fentanyl and carfentanil.
None of these drugs has yet been commercialized, however. One was licensed to a big pharmaceutical company but withered on the vine. The problem, Janda says, is that addiction, even in the world of pharmaceutical development, carries a stigma—a pervasive feeling that it is a moral failure rather than a brain disease. It doesn't help that nobody has ever successfully made a vaccine for addiction, or that Big Pharma doesn't see it as particularly profitable.
Just as the fight seems almost hopeless, however, it appears that Janda's quest for a silver-bullet for addiction may not have been Quixotic after all. A new generation of scientists—some schooled in Janda's lab—may soon deliver potent new weapons in the battle for the addict's brain.
Arms Race
There's a desperate need for new weapons to fight for the lives of the 494,000 Americans over the age of 12 who are regular heroin users, the 15 million Americans who regularly abuse prescription drugs, the 774,000 Americans who regularly use meth and the 5 million Americans who regularly use cocaine. As big pharma has engineered more and more powerful opioids, and drug cartels have sought to exploit these advances to make more money, scientists and public health advocates have been racing to develop countermeasures aimed not just at fighting addiction, but also at saving lives.
For a brief period, they seemed to be making genuine progress. In 2018, drug deaths in the U.S. declined for the first time in 25 years. Sadly, those gains have proved fleeting. Last month the CDC reported that nearly 72,000 Americans, or 197 people a day, died from drug overdoses in 2019, an increase of 5 percent over 2018 and a new record, according to numbers released last month by the CDC. "We had started to see some pretty positive turns of events and it seemed as though we'd finally gotten to the top of this terrible mountain of drug overdoses and deaths," says Ryan. "The problem was we hadn't yet come all the way down."
There's a factor in addition to the pandemic driving the resurgence of the overdose crisis: the decision by the Mexican drug cartels to mix deadly synthetic opioid adulterants into the drug supply. Though fentanyl was present on and off in the early 2000s, in the last few years it's become a staple. The effect has been devastating. Fentanyl is more than 50 times stronger than heroin. It's almost impossible for the street-level user to gauge its potency. Ryan estimates that 90 percent of patients he treats for opioid disorders nowadays have used fentanyl.
Mixing in fentanyl, or even selling it outright, can be lucrative. A kilogram of heroin can produce 10,000 doses; a kilogram of fentanyl, analysts estimate, will produce 500,000. Until recently, however, production of the precursors of the drug was limited to a handful of labs, most of which U.S. law enforcement authorities, in collaboration with their Mexican counterparts, were able to identify and take out. In recent years, labs have sprung up in China to supply the market in North America, which makes it hard for U.S. law enforcement to discourage production.

"We have much less ability to go to China and say, 'Hey, we know you've got a chemist producing something that's killing Americans, take care of it'," says Jonathan Caulkins, a fentanyl expert and professor at Carnegie Mellon University who coauthored a Brookings Institute Report on the opioid epidemic published in June. "There are now an unlimited number of people who are capable of doing that kind of chemistry," he says. "Illegal markets have a minimum buyable operating size. If they're below that size, they can be snuffed out. Once they're above that size, then they are sustainable and essentially never disappear. I'm afraid that with fentanyl, the horse is now out of the barn."
As if that weren't bad enough, the cartel has also flooded the U.S. market with new, extremely potent forms of methamphetamine. "Something that has been clear for decades is that when potency goes up and price goes down, more addicted people who are using drugs die," says Andrew Kolodny, the founder and executive director of Physicians for Responsible Opioid Prescribing (PROP), and medical director of opioid policy research at Brandeis University's Heller School for Social Policy and Management. "The reverse is true as well, when the price goes up and the potency goes down, that could drive more people who are addicted to seek treatment. They start to run out of resources."

Big Weapon
The pandemic has had one silver lining, prompting some policy changes that have helped addicts. For instance, most methadone clinics have long required addicts to physically appear daily to get their medication. That was challenging even during normal times, when an otherwise harmless bout of laziness could snowball into uncontrollable drug cravings, relapse, overdose and death. Recently, however, the U.S. Department of Health and Human Services began allowing clinics to issue a month of methadone supply at once, which could make a huge difference, Volkow says.
Similarly, until recently doctors were required by law to see patients in person and take a full history prior to prescribing buprenorphine, the most widely used opioid medication. This had long proven a barrier for patients in rural areas with limited access to health care. The DEA now authorizes doctors to issue the drug through telehealth appointments. These efforts could lead to real improvements in the months ahead.
In a few years, addicts may finally benefit from the research that Janda started so long ago. Two of Janda's former graduate students, Paul Bremer and Nicholas Jacob, recently joined Cessation Therapeutics, a private company founded in 2018 to commercialize some of his technologies, including vaccines and antibodies for addiction.
The company is taking advantage of the fruits of Janda's early work. For instance, in the case of the vaccines, Janda uses synthetic organic chemistry to take opioid and other drug molecules and graft them onto larger compounds that are easy for the immune system to recognize. That neutralizes the advantage of small size, which normally allows drug molecules to pass unnoticed by the immune system. Once a doctor injects this hybrid drug into the body and the addict's immune system recognizes it as "foreign," it begins to create antibodies that seek out and eliminate the drug. To the addict, that blunts any high.
Over time, these antibodies help to reduce addiction. "When vaccines and antibodies interfere with a high, they create a memory," NIDA's Volkow explains. "The brain learns that a drug that, in the past, released a high, no longer does. It basically erases the association with pleasure. So with repeated exposure, it can overcome the initial memories and help extinguish them."
The vaccines have a key limitation: they need months to take effect. It takes that long for the body to build up immunity, and usually two or three booster shots, typically a month or so apart, are needed. When antibody levels are low, the drugs pack such a potent punch that drug addicts can simply overpower the body's existing store of antibodies. During this time, an addict may relapse and disappear from treatment, failing to follow through with booster shots. "The problem with addicts is they're not going to wait," Janda says.
It's also not clear whether or not a vaccine would provide robust protection. If a vaccine doesn't trigger the production of a sufficiently high level of antibodies, opioids or other drugs may be able to vanquish them. This question, researchers hope, will be answered in phase-three clinical trials.
These limitations, coupled with the recent surge in overdose deaths, have prompted Janda and others in the field to consider so-called "passive immunizations"—the direct injection of lab-synthesized antibodies, which can be administered in huge quantities. These antibodies soak drug molecules up "like a sponge" as soon as they are administered. Although such antibodies are expensive and only last several weeks, they provide immediate protection against both a drug high and an overdose. Antibodies could buy newly-vaccinated addicts time for their immune systems to kick into gear.

Antibodies could prove particularly useful in the case of carfentanil. Although this drug's synthetic opioids attach to the same brain receptors as heroin, the anti-overdose drug Narcan isn't always effective against them. That's largely because the synthetic drugs have a longer half-life in the body than Narcan. Patients treated with Narcan for overdoses caused by batches of heroin adulterated with some synthetic opioids can overdose a second time when the Narcan begins to wear off, go into respiratory depression and die. "With the monoclonal antibody, you don't have that issue," Janda says. "As soon as you put it on board, you're fully protected. The antibodies should stay around for several weeks."
Cessation Therapeutics hopes to begin human trials for a carfentanil antibody, which has already been shown to be effective in mice and nonhuman primates, in the next 12 to 16 months.
Another group of scientists, from the University of Arkansas and biotech company InterveXion, have produced a monoclonal antibody that targets methamphetamine. It recently entered phase-two clinical trials. "If it's successful, it will be the first time we have a treatment to reverse toxicity from methamphetamines," says NIDA's Volkow. "I'm very excited about the possibilities for passive immunizations. It's very promising."
If all goes well, antibody treatments will begin to hit the market over the next few years; eventually, with luck, vaccines may follow, giving clinicians potent new weapons against the ravages of drug abuse. As COVID-19 adds to the ranks of the addicted, there's no time to lose.
- Get link
- X
- Other Apps

Comments
Post a Comment